Nudge or name-and-shame? How do we reduce variability in the system? #ClinicSpeak #MSBlog
Earlier this week I mentioned that I was appalled by the observation that where you live in the country and how your local MS service is configured determines how quickly you can access DMTs.
In one English town all patients had to be referred to a regional neuroscience centre taking on average 9 months to get onto a DMT, whereas in another similar-sized town with a local MS service patients managed to get onto treatment within 8 weeks. Does this make a difference? In this US electronic health record study patients who initiated DMTs later, i.e. > 3 months after being diagnosed with MS, were more likely to have a relapse than patients starting DMT within 3 months. Time matters!
Some people may say that as MS is a lifetime disease a short delay is neither here nor there in the grand scheme of things. I disagree. For every relapse their is ~10 white matter MRI lesions that occur asymptomatically. For every visible white matter lesion there is over 25 microscopic white matter lesions that the pathologists will see under the microscope. As we now know MS is as much a gray matter disease as a white matter disease how much activity are we missing in the gray matter. Therefore one relapse indicates that a lot more damage is occurring that meets the eye. This is why I continually push the issue of Time Matters in MS. It is also important to realise that once damage occurs in MS it is generally irreversible and that if recovery occurs it is due to plasticity and other compensatory mechanisms. Once we exhaust these recovery mechanisms worsening MS become clinically apparent (formerly known as progressive MS).
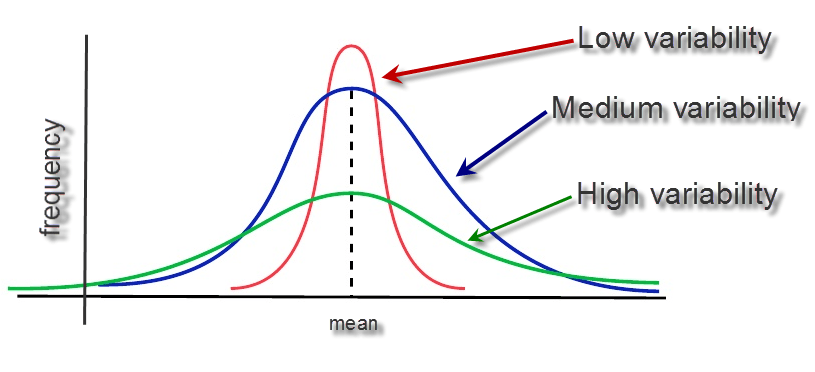
How do we reduce the variability in the healthcare system when it comes to the management of MS? Do we name and shame units? Do we educate and help them? Do we ask patients to vote with their feet? Do we provide them with resources and know-how? Do we gently nudge them to change their local practice? There is no easy answer, but for the sake of people with MS we need to change the way we do things. Excessive variability in a system suggests something is wrong. Help!
Corvino et al. The association of timing of disease-modifying drug initiation and relapse in patients with multiple sclerosis using electronic health records. Curr Med Res Opin. 2017 Mar 20:1-14.
OBJECTIVE: A large, US de-identified electronic health record (EHR) database (Optum-Humedica de-identified Electronic Health Record dataset) was used to evaluate whether earlier disease-modifying drug (DMD) treatment initiation was associated with improved outcomes in MS.
METHODS: Newly diagnosed patients from 1/1/2008-8/30/2014 (International Classification of Diseases, Ninth Revision, Clinical Modification code: 340.xx; first MS diagnosis = index date) with healthcare activity 1 year pre- and 2-years post-index, and who initiated DMD treatment during the 2-year follow-up period, were included. Patients were categorized as Early or Late Initiators (initiated DMD treatment ≤90 or >90 days following index, respectively). Relapse was determined by the presence of an MS-related hospitalization or an outpatient encounter with MS diagnosis and corticosteroid prescription within 7 days.
RESULTS: A total of 4,732 patients met the inclusion criteria: 2,042 (43.2%) were Early Initiators and 2,690 (56.8%) were Late Initiators. Similar baseline mean age (46.9 years for both cohorts) and Charlson Comorbidity Index scores (Early Initiators: 0.3, Late Initiators: 0.32) were observed. Average time to treatment was 20.9 ± 27.6 days for Early Initiators and 346.3 ± 181.1 days for Late Initiators. A significantly higher proportion of Late Initiators (n = 609; 22.6%) had a relapse during the 2 years following MS diagnosis compared with Early Initiators (n = 403; 19.7%; p = 0.0158). After controlling for covariates using multivariable logistic regression, Late initiation of DMD treatment was associated with greater likelihood of relapse compared with Early initiation (odds ratio 1.189; 95% CI: 1.031-1.371; p = 0.0172).
CONCLUSIONS: Later initiation of DMD treatment (ie, >90 days after MS diagnosis) in patients with MS was associated with a greater likelihood of relapse compared with earlier initiation. Early initiation of DMD treatment following a diagnosis of MS may have an effect on long-term outcomes.
CoI: multiple